
How to Find the Best Knee Surgeon
Learn what to look for when finding the best knee surgeon. The tips to consider when searching, such as cost, experience & much more.
A Review of a Retrospective Study

This article is aiming to investigate whether low BMI status increased the risk for two year mortality, or reoperation 90 day readmission, or extended length stay following total joint arthroplasty (source abstract).
As a surgeon, I’ve always been concerned about the potential risk of low body mass index patients in total joint arthroplasty. Honesty, even more than overweight patients, especially for wound issues such as, wound healing and wound drainage.
Malnutrition is a devastating condition, which disproportionately affects the elderly population. Malnutrition furthers the pre-existing risk of osteoarthritis in these patients and exacerbating joint damage, furthering the need for total joint arthroplasty.
A marker of malnutrition is a low body mass index. This retrospective study was performed using the partner arthroplasty registry, which contains data from 2016 to 2019 in nearly 5,000 primary total hip and knee arthroplasty patients.
Malnutrition is a devastating condition, which disproportionately affects the elderly population. Malnutrition furthers the pre-existing risk of osteoarthritis in these patients and exacerbating joint damage, furthering the need for total joint arthroplasty.
Underweight BMI was found to be independently associated with increased risk of mortality and length of stay. BMI was analyzed as a categorical variable with the following level as defined by the centers for disease control and prevention (CDC).
Underweight patients were defined as those with less than 20 (44 lbs) kilograms per square meter.
Following univariable analysis, our outcome variables mortality and length of stay were found to be significantly different between underweight and normal BMI code.
Whereas 90 day readmission and reoperation rates were similar between groups. After accounting for potential confounders of gender and joint type, underweight BMI was found to be independently associated with increased risk of mortality within 2 years following total joint arthroplasty.
Among their patient population, underweight patients face an 18-fold increased risk of 2 year mortality compared to patient in the obese class 3 code, when accounting for joint type and gender; seems interesting.
When BMI was assessed continuously, decreasing BMI was significantly associated with increased risk of 2 year mortality. Specifically, a 1 kilogram per square meter decrease in BMI was associated with a 9% increased risk of 2 year mortality following total joint arthroplasty.
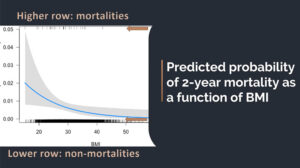
This figure illustrates the predicted probability of 2 year mortality as a functional BMI was corresponding to a 95% confidence interval. The vertical tick marks indicate individual patients with the higher route representing mortalities, and the lower representing non-mortalities.
Among their patient population, underweight patients face an 18-fold increased risk of 2 year mortality compared to patient in the obese class 3 code, when accounting for joint type and gender; seems interesting.
The others suggest that although BMI is a validated indicator for malnutrition, serum albumin, cholesterol, and urinary creatinine levels are also indicative of this condition and further studies should be conducted to initiate the relationship between the preoperative levels of these markers in patients.
The findings of the study demonstrated that total joint arthroplasty patients with an underweight BMI experienced an 8 times increased risk of 2 year mortality and an increased length of stay of 0.44 days.
The article suggests that orthopedic surgeons should consider nutritional consultation and medical optimization in this high risk patient prior to surgery.
As a result, these patients and their providers need to carefully assess risks and benefits of total joint arthroplasty and decide whether it is the best option for the patient.

Learn what to look for when finding the best knee surgeon. The tips to consider when searching, such as cost, experience & much more.
Having total knee replacement surgery can seem intimidating. So read these 10 tips to prepare for knee surgery and be on your way to a smooth recovery.

There are many reasons why patients put off knee surgery. Learn more about other treatments & the consequences of waiting too long for surgery.